

6, 7Ĭhronological age alone provides relatively little information regarding the tolerance of older patients to cancer treatments. 4, 5 Moreover, quality of life (QoL) and functional endpoints are not well represented in clinical trials and should be considered at least as relevant as overall survival (OS). 2, 3 This risk is also influenced by the increasing burden of comorbidities and polypharmacy, which increase the risk of adverse events and also impact survival.
1 The multi-organ age-related decline can alter drug pharmacokinetics and increase the risk of complications of locoregional and systemic treatments. More than half of all patients with non-small cell lung cancer (NSCLC) are aged above 70 years, and almost 10% are 80 years or older. This article provides a detailed review of these immunotherapy agents with a focus on the data available regarding older NSCLC patients and makes recommendations to fill evidence gaps in this patient population. However, most of the data available from these trials are derived from, and therefore might be more applicable to younger and fitter patients rather than older and often frail lung cancer real-world patients. Following the successful introduction of single-agent immunotherapy, current clinical trials are focusing on combination treatments with chemotherapy or radiotherapy or even other immunotherapeutic agents. This approach has resulted in improved survival and a more favourable toxicity profile when compared with chemotherapy.
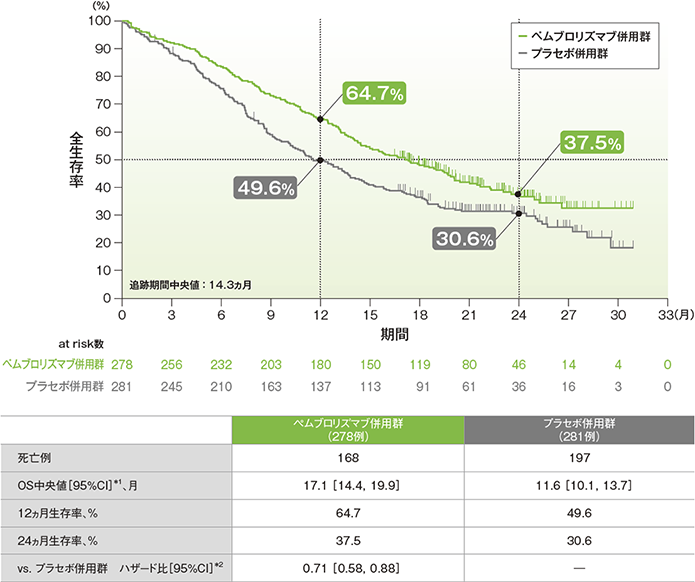
Immunotherapy with checkpoint inhibitors against programmed cell death receptor (PD-1) and programmed cell death ligand (PD-L1) has been implemented in the treatment pathway of patients with non-small cell lung cancer (NSCLC) from locally advanced disease to the metastatic setting.


 0 kommentar(er)
0 kommentar(er)
